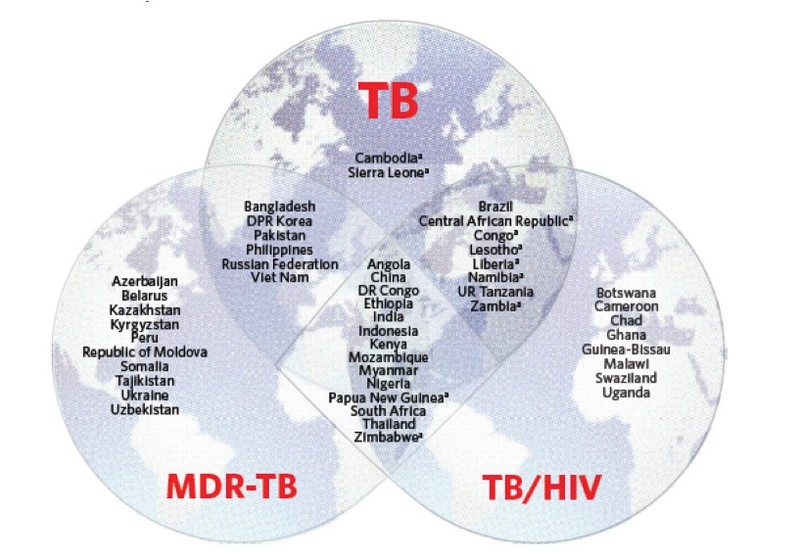
30 HIGH TB-BURDEN COUNTRIES
The WHO has defined three lists of high TB-burden countries for the period 2016-2020 to differentiate the various forms of the disease - tuberculosis, TB/HIV co-infection and multidrug-resistant tuberculosis (MDR TB). Each list contains 30 countries with high TB rate and emphasizes global actions and commitment needed to fight against TB. Given overlap among the lists, 48 global countries are on at least one list and 14 countries are on all three lists.
LACK OF ACCURATE DIAGNOSTICS
In many developing countries, the conventional method of diagnosing tuberculosis is smear microscopy that is only 20-60% accurate depending on the resources available and the skills of technicians. This method may be precise when operated under the right conditions (when a sample is diagnosed as “TB positive” by microscopy, it is almost always a true positive). But many true positives can be missed if conditions are not met. Constrained resources are prevalent in regions that tend to have a high TB burden

TB AND HIV
Tuberculosis and HIV often go hand in hand and form a lethal combination, each disease accelerating the progress of the other. Accordingly, tuberculosis is the major cause of serious illness and death among HIV positive individuals worldwide. HIV also makes tuberculosis difficult to diagnose and to treat among people living with HIV.
At least one-third of people living with HIV are infected with TB bacteria each year. People living with HIV are at 20 to 30 times higher risk of contracting/developing active TB than people without HIV.
About 35% of people with HIV die due to tuberculosis and a quarter of TB deaths are among people with both tuberculosis and HIV
STIGMA
Due to the close association between tuberculosis and HIV, many sufferers experience stigma, discrimination and exclusion from their families and communities. Lower quality of life, depression and deteriorating social relationships occur in addition to the impact on physical health.
The fear of being stigmatized and “found out” causes many tuberculosis or HIV sufferers to delay testing or skip or even quit treatment. As a result, the disease continues to progress, becoming serious while infecting others and challenging control of the disease.
APOPO works with volunteers groups to help sentitise communities and fight against stigma.


SLOW RATE OF DECLINE
TB incidence has decreased by an average of 1.5% since 2000. According to WHO estimates, the decline is too low to meet the target set by the WHO’s “End TB Strategy”, which requires 4 to 5 percent rates of annual declines by 2020. What is needed is a fast and accurate mass-screening tool. Working alongside conventional methods as an “add-on” technology, APOPO aims to make its HeroRATs the standard “go-to” tool for quickly increasing tuberculosis detection rates at health clinics.
STORIES: BENNY
“I went to clinic three times and no-one knew why I was ill. Then APOPO identified my TB.”
